Atopy
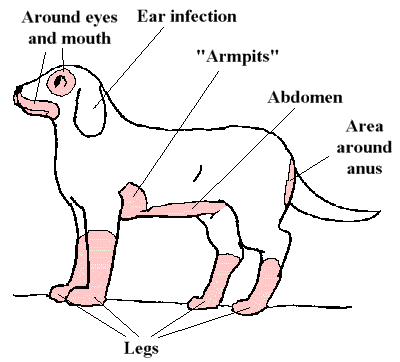
Food allergies tend to affect these areas. Graphic by MarVistaVet
Everyone knows someone with hay fever. Airborne pollens, molds, dust particles, etc. are inhaled and soon the sneezing and sniffling begins. A simple way to think of atopy for pets would be saying that the airborne allergen is inhaled by the pet but instead of sneezing and sniffling, the pet gets itchy skin. In fact, this was what we thought was happening for many years, but the situation turns out more complicated.
In atopic dermatitis, airborne pollens, molds, dust particles etc. gain entry to the skin through a defective skin barrier. Inhaling is not involved. The immune system becomes inflamed by the airborne allergens and soon the itching and scratching begins. The allergens come from the air, but the itch is felt in the skin.
Airborne particles (pollen, dander, etc.) are harmless to someone who is not allergic to them. Allergy develops in individuals who are genetically programmed to do so.
Breeds predisposed to develop atopy include: Dalmatian, Golden retriever, West Highland white terrier, Shar Pei, Labrador retriever, Cairn terrier, Lhasa Apso, Shih Tzu, Boxer, and Pug.
Features of Atopy in Dogs
There are many reasons for pets to itch: parasites, allergy to flea bites, food allergy, secondary infection and the list goes on.
The following are findings in the history and examination of the patient that might lead to a diagnosis of atopy. In fact, meeting five criteria from this list yields an 85 percent accuracy for the diagnosis of atopic dermatitis, at least for dogs:
- Young Age of Onset
Seasonal itchiness due to atopy tends to begin early in a pet’s life (between ages 1 and 3 years in 70 percent of dogs diagnosed with atopy). Food allergy tends to begin later (more like age 5 or 6 years in dogs) or earlier (less than 6 months of age). Age at which itching first manifests is not as reliable a sign in cats as in dogs. - Mostly Indoor Lifestyle
It is indoors where many airborne allergens concentrated; however, it is important to note that allergens in the air are in the air for miles so it is not easy to escape allergens by simply going outdoors nor by simply going indoors. - Good Response to Steroids
Whether the patient is a dog or cat, itchiness due to atopy responds rapidly to cortisone-type medications (prednisone, betamethasone, dexamethasone, etc.) as does itching due to insect bite allergy. Food allergy is more variable in its response; it may or may not respond well. - Chronic or Recurring Yeast Infections in the Skin
Yeast (Malassezia pachydermatis) live on the surface of the skin normally but with all the changes allergy causes to the skin’s microenvironment, yeast will proliferate and create a stinky, thickened, pigmented skin that resembles elephant skin or even tree bark. Environmental allergy is a strong predisposing factor in developing yeast dermatitis. - Front Feet Involved
Whether it is chewing the top of the feet or between the toes, foot licking is a classic feature of atopic dermatitis. - Ear Flaps Involved
The non-haired (inside) portion of the ear flap (the concave pinna) is commonly involved in atopic dermatitis regardless of whether the inflammation extends down the ear canal and leads to what we usually think of as an ear infection. The concave pinnae become greasy, red, thickened, smelly or any combination of the above. - Ear Margins Not Involved
Ear margin involvement is suggestive of sarcoptic mange and would lead one away from airborne allergies. - Lower Back Area Not Involved
The lower back is the flea bite zone. There are few conditions other than flea bite allergy that cause itching in this area, so if this area is involved, make sure flea control is achieved before further evaluating the skin. - Seasonality
Seasonality of the itching is also a clue towards an airborne-related allergy, but since there are many climates where seasons are ambiguous, this is not necessarily a hard and fast feature of atopic dermatitis. It should also be noted that while skin testing and blood testing are used to make immunotherapy sera to treat atopic dermatitis, reactions and positive results on these tests do not contribute to making a diagnosis of atopic dermatitis. Many normal animals will have positive results. These tests are for animals where the diagnosis of atopic dermatitis has already been made based on the above criteria as well as ruling out other itchy diseases.
There is no Test for Atopic Dermatitis
Unlike other diseases where a test of some sort can be performed, atopic diagnosis is a clinical diagnosis, which means the diagnosis is made based on symptoms and findings such as those listed above. Allergy testing, which is done either by skin test or by blood testing, is not a test for atopic dermatitis; instead this type of testing is done after the diagnosis has been confidently made based on findings in the patient. Allergy testing is conducted to determine how best to make an allergy shot serum for a specific patient; it is not part of disease diagnosis.
In cats, the irritation pattern is not as characteristic. There are four common manifestations of atopy. Unfortunately, these same irritation patterns can be found in numerous other skin conditions and, in fact, up to 25 percent of atopic cats have multiple types of allergies.

Non-lesional fur mowing. Photo by MarVistaVet
Treatment Options
Many people are frustrated because treating atopic dermatitis focuses on controlling the symptoms. Unfortunately, finding out what a pet is allergic to is not entirely possible and even when it is, because pollens and other material circulate in the air for miles, you can’t just avoid allergens in the air. Only hypersensitization treatment stands a chance at actually changing the patient’s immune system so that they are no longer allergic, but this is far from a sure thing. The good news is that at the end of the day, the goal is healthy comfortable skin and there is a lot that can be done towards achieving this. How big a project this becomes depends on an individual patient’s ability to respond to different therapies or combinations of them. Here are some of the options.
Clearing Secondary Infections
Before doing anything else, it is important to clear up secondary infections. Secondary infections involve bacteria (usually Staphylococcal) and/or yeast (Malassezia) at the site of the itchiest areas on the body. These organisms live naturally in the skin but when the skin is irritated, they gain access to inner tissue layers and proliferate. Sometimes they actually come to generate further allergic response in the skin. These infections tend to recur and are the usual cause of recurrence of itch symptoms in a patient who was previously controlled.
Hyposensitization (Allergen Specific Immunotherapy)
Hyposensitization, more commonly known as allergy shots, is by far the treatment of choice for atopic dermatitis. All the other medications are basically just itch relief; only hyposensitization actually changes the immune system. Some dogs are eventually able to go off all treatment and are no longer allergic after they have been on hyposensitization long enough. Most dogs experience at least enough improvement to require fewer additional treatments but there are some caveats before making an appointment for allergy testing.
- Allergy shots require approximately 6 to 12 months to begin working.
- 25% of atopic dogs will not respond (these are usually the animals allergic to multiple allergens).
- 25% will require prednisone or similar steroid at least at some times.
- You will most likely have to give the allergy shots yourself.
- Referral to a veterinary dermatologist may be necessary.
In hyposensitization the patient is injected with small amounts of allergens on a regular basis. As time passes, the amounts of allergens increase and injections are given at longer intervals. The selection of allergens is made based on the results of either an intradermal skin test (as described above), an in vitro test (a blood test) or a combination of the results of both tests. The younger the pet is when this treatment starts, the better it works.

Reactive blebs. Photo by Dr. Mitch Song.
Steroid Hormones
These cortisone-type medications (prednisone, prednisolone, triamcinolone, dexamethasone, etc.) have been useful as the first line of defense against itchy skin for decades, and they are still widely used. There are negative side effects with higher doses as well as with long-term use, so the trend is to use other medications to either remove the need for steroids or reduce the amount needed for itch control.
Side effects include:
- Excess thirst
- Excess hunger
- Excess urination, which could lead to house-breaking issues
- Suppression of the immune-system/bringing out latent infection, especially urinary tract infection and upper respiratory infection.
- Raising blood sugar/destabilizing a borderline diabetic (especially a problem for cats if long-acting injectable steroids are used). In the short term, side effects can be controlled by adjusting dosage but in the long term, these medications are more problematic and if possible their use should be minimized.
Steroid hormones are useful for acute flare-ups as well as for long-term management of atopic dermatitis (assuming limits are placed on how long they are used). Side effects are greatly minimized when steroids are used topically.
Cyclosporine
Cyclosporine is a modulator of the immune response that has been helpful in both human and non-human organ transplant patients. It has been found to be reliably effective in atopic dermatitis and does not carry the unpleasant side effect profile that steroids do. That said, it is not without side effects of its own. It is used mostly in dogs but can also be used in cats. It is for long-term management and is not helpful for acute flare up control.
Oclacitinib (Apoquel)
This is a new medication best used for itching relief and blocking itch symptoms. Apoquel is popular as it works fast. It does not address the inflammation in the skin; it just stops the itch sensation. This means that any skin infection causing the itch will still need to be controlled.
Canine Atopic Dermatitis Immunotherapeutic (Cytopoint®) Injections
This is a new treatment that uses vaccine technology to eliminate one of the main mediators of itch sensation. The injections provide relief from itching for one month in 80% of dogs (many dogs get longer relief) and usually show effectiveness within 24 hours.
- Bathing the pet weekly to remove allergens from the fur may be helpful in reducing allergen exposure, plus tepid water is soothing to itchy skin. There are also many therapeutic moisturizing shampoos that can be used to restore the skin’s natural barrier or to assist in general itch relief.
- Avoid stuffed toys, wash bedding regularly. This minimizes dust mite exposure. Also, remove the pet from the area when vacuuming or dusting.
- Use air-conditioning and/or an air filter system.
- Keep the pet away from the lawn while it is being mowed.
- Minimize houseplants.
Omega 3 Fatty Acid Supplements
These products are not analogous to adding dietary oil to the pet’s food, such as olive oil, coconut oil, corn oil etc. Instead, these special fatty acids act as medications, disrupting the production of inflammatory chemicals within the skin. By using these supplements, it may be possible to postpone the need for steroids/cortisones or reduce the dose of steroid needed to control symptoms. It takes a good 6 weeks to build up enough omega 3 fatty acids in the body to see a difference.
Ultra-Microsized Palmitoylethanolamide or PEA (Redonyl®)
Plants and animals make a natural substance called PEA. In animals, it helps restore balance to the skin’s biochemistry and prevents release of the biochemical causes of itching. The commercial product uses a soybean extract to obtain its PEA and creates a super concentrate as it would not be possible to eat enough soybeans to get a therapeutic dose of PEA. The super small ultra-micronizing allows it to be absorbed better. It is available as a flavored chew for dogs and can also be used in cats.
Antihistamines
Antihistamines have been popular for many years for pets, and it seems their effectiveness does not stand up to scrutiny. They provide neither short-term relief nor reliable long-term relief. They may be helpful in combination with other products in that their use may reduce the need for other products. They may work better in cats than in dogs.
Solid Flea Control
Allergies are additive. This means that when a patient has multiple allergies, each allergy alone may not be enough to cause itching but the allergies all active together probably will. Consequently, taking away one of the active allergies may be enough to allergy reduction to resolve the itching. Flea bite allergy is extremely common. We now have so many effective products available that there is no reason for an animal to contend with a flea bite allergy. This simple bit of therapy (flea control) may be enough to bring the pet below her itch threshold without having to contend with any of the therapies listed above.
Itchy skin has been the scourge of dogs, cats and their owners for decades, if not centuries. We are now armed with a great understanding of immunology and have many tools to address allergy symptoms. Your veterinarian can guide you further with regard to a proper regimen. If your veterinarian decides treatment is not working as well as hoped, discuss whether or not a referral to a veterinary dermatologist is in your pet’s best interest.

